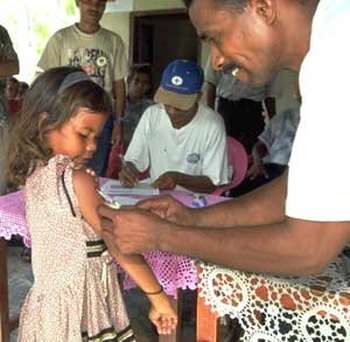
Vaccin inde
Smallpox or smallpox is an infectious viral disease, highly contagious and epidemic, caused by a poxvirus. It has been totally eradicated October 26, 1977 (last known case in Somalia, a hospital cook), thanks to a campaign by the World Health Organization (WHO) combining mass vaccination campaigns, in 1958, with a ‘strategy of surveillance and containment’, implemented from 1967. Today only samples of the virus are preserved for research by laboratories approved by WHO.
The word smallpox comes from the Latin varus, i (which means pustule) and varius, a, um (meaning spotted). Indeed, smallpox is characterized by a sort of ‘stippling of pustules.’
After 1980
Officially, two strains were kept for research at the Center for Disease Control (CDC) in Atlanta (USA) and the State Institute of Virology and Biotechnology in Koltsovo (Russia).Both laboratories were initially developed for germ warfare during the Cold War. Recently, and particularly following the anthrax attacks in the United States in 2001, some institutions have highlighted the possible use of smallpox as a biological weapon.
In 1999, a committee of the WHO announced that the reserves of available vaccines are too limited and must boost production of vaccines. A survey by WHO in 1998 estimated the number of doses available worldwide at 90 million.
Therefore, the United States, France and other countries have boosted the production of vaccine against smallpox, especially after the attacks of September 11, 2001 attacks and the anthrax. In France, a ‘governmental plan for mass vaccination against smallpox’ provides, in the event of a recurrence of the virus, a device for vaccinating the entire population in 14 days in units of basic vaccination (UVB) spread over the territory.
Fight against smallpox
The story of the fight against smallpox can be divided into three periods: the first phase of inoculation, then that of vaccination, and finally that of the global eradication campaign (1958-1977).
Variolation
In India, smallpox is described in Ayurvedic books. The cure ayurvedic passed by the inoculation of a ‘smallpox material’ one year old, from pustules of people who contracted smallpox in the previous year. The effectiveness of this method was demonstrated by the British physician JZ Holwell in a report to the College of Physicians in London in 1767.
The first written mention of smallpox comes from a doctor in Alexandria, Aaron. From the eleventh century, the Chinese played variolation: it was hoped to inoculate a form that few virulent by contacting the person to be immunized with the content of the substance suppurating blisters of a patient . The Prime Minister Wang Dan, who after losing a son of smallpox had convened a variety of practitioners from all over China to develop prophylaxis.A Taoist monk brought the inoculation technique which spread gradually throughout China.
The result, however, remained uncertain and risky, the mortality rate could reach 1 or 2%. The practice has gradually spread along the Silk Road. In 1701, Giacomo Pylarini made the first inoculation in Constantinople.
The technique is imported in the West in the early eighteenth century by Lady Mary Wortley Montagu, wife of the ambassador from Britain to Turkey, who learns of Dr. Emmanuel Timoni (ca 1670-1718), physician to the embassy of Great Britain in Istanbul. A graduate of the University of Padua, a member of the Royal Society of London since 1703, Dr. Timoni published in 1713 in the Philosophical Transactions of the Royal Society his treatise on inoculation. His work has reissued the following year at Leipzig. From that date, the literature on this subject is increasing, Pylarino in 1715, Leduc and Maitland in 1722 … It was introduced in France later.The first truly mediated inoculation is conducted by Dr. Theodore Tronchin in 1756 on children of the Duc d’Orleans. In 1760, Daniel Bernoulli showed that, despite the risks, the spread of this practice would save a little more than three years of life expectancy at birth. However, it aroused the hostility of many physicians.
Jenner’s vaccination
For the first time, the 1770s until 1791, at least six people were tested, each independently, the possibility of immunizing human smallpox by inoculating them with cow pox, which was present on the udder cow. Among those who made the first tests are in 1774, an English farmer Benjamin Jesty on behalf of, and in 1791, a German schoolmaster named Peter Plett. In 1796, the English physician Edward Jenner will make the same discovery and fought so that we formally recognize the good result of immunization.14 May 1796, when he inoculated a child of pus on the hand of a farm infected with vaccinia (via contact with infected cow’s udder) or smallpox cows (cow pox ‘in English) . Three months later, he inoculated smallpox in the child, who resisted, thus revealing themselves immunized against the virus. This practice then spread gradually throughout Europe. Nevertheless, smallpox remained endemic throughout the nineteenth century and has gradually disappeared from Europe after the First World War.
For the record, the vaccination at that time was to remove pus from the pustules and directly infect humans with (do not forget that Louis Pasteur and asepsis came only later). And rather than carrying a cow infested, it was easier to move with a man recently ‘vaccinated’ and who had pustules.
Total eradication of smallpox
In 1950 the Pan American Health Organization, based on a novel method developed by Collier, undertook to eradicate smallpox in the Americas (this will be achieved in 1967 (except Brazil).
The Soviet Union moved in 1958 to fully eradicate smallpox, which was then 2 million people per year worldwide. The project was taken that year by the World Health Organization (WHO). The original strategy proposed by the USSR, an estimated vaccination rate of 80% would be enough to eradicate the virus. The vaccination campaign nevertheless proves difficult to implement.
The final report of the Global Commission for the Certification of the Eradication of WHO noted: ‘The eradication campaigns based entirely or mainly on mass vaccination was successful in some countries but failed in most cases. […] In India, five years after a national campaign to eradicate business 1962 (55 595 cases), the number of notifications was larger (84 902 cases) than it had been since 1958.It would have been extremely costly and logistically difficult if not impossible, to achieve much higher levels of coverage. With the resources available, it was absolutely necessary to change strategy. ‘
WHO changes its strategy in 1967, implementing the ‘strategy of surveillance and containment’, which is to isolate cases and to vaccinate all those who lived around epidemic outbreaks. An international team formed under the leadership of the American Donald Henderson.
The eradication campaign was met first at the problem of identifying outbreaks, all is not necessarily identified. The social, cultural and political also played an important role. In India and Bangladesh, many Hindus were opposed to vaccination for fear of offending Shitala Devi, the goddess associated with smallpox. In addition, one year, heavy rains during the monsoon broke the dams and dykes, forcing people to flee, which had the effect of extending the new outbreak, which was eradicated at the end of one year of effort.Sudan, he was plunged into civil war, exposing health teams with increased risks (which did, however no casualties to deplore).
The last major European outbreak of smallpox occurred in 1972 in Yugoslavia. A young Kosovar returning from a pilgrimage to Mecca and Iraq caught smallpox. The epidemic affects 38 people, including 6 die. The Tito regime then declared martial law, imposed quarantine and began a massive campaign of re-vaccination of the population, with the assistance of WHO and the team from Henderson. The epidemic was curbed in two months. A few years ago, another source of infection was reported in Sweden (May-July 1963). This was also eradicated through quarantine and vaccination.
The last case of spontaneous severe form of smallpox (Variola major) was recorded in Bangladesh in October 1975 with a girl two years, Rahima Banu. From this date, smallpox was considered eradicated in virtually all the world, with the exception of the Horn of Africa.Indeed, poor health infrastructure and roads in Ethiopia and Somalia made it very difficult to mass vaccination had been successful elsewhere. In addition, there also armed conflict, famine and migration of refugees which further complicated the task. Nevertheless an intensification of vaccination measures, surveillance, containment, in early 1977, the last case of smallpox was diagnosed in a natural way in Merca in Somalia, October 26, 1977.
After eradication
Although smallpox no longer Circulate in the human population, some medical laboratories had kept stocks of variola virus. However, in August 1978, Janet Parker, a photographer from the School of Medicine, University of Birmingham came to the hospital with symptoms of smallpox. Serologic tests confirmed her condition and she died Sept. 11 of that year as a result of the disease. Professor Henry Bedson, head of research on smallpox in this laboratory committed suicide shortly after.
Therefore it was decided that all known stocks of the virus would be destroyed or transferred to one of two laboratories accredited by WHO, the Centers for Disease Control and Prevention (CDC) United States and the Centre National de Recherche Virology and Biotechnology (VECTOR) Koltsovo, USSR. In 1986, WHO recommended that eventually the complete destruction of these viruses for December 30, 1993. But after an initial postponement to June 30, 1995, the decision was postponed and then canceled in 2002. Even if the total destruction of stocks reduces the risk of an accident leading to a new outbreak of disease, these viruses can be useful for biomedical research and for development of new vaccines, antiviral drugs, etc. .
In March 2004, samples of smallpox virus were discovered in Santa Fe in an envelope inserted between pages of a book of medicine dating from the Civil War; These samples are being analyzed by the CDC to understand the history of smallpox during the centuries.
Medical treatment of meningitis
Antibiotics.Usually penicillin G, ampicillin, chloramphenicol or ceftriaxone, depending on the bacteria identified. Antibiotics in early treatment of meningitis are effective to stop the disease and reduce the rate of mortalité3. According to the U.S. Agency Center for Disease Control and Prevention, appropriate antibiotic treatment reduced to less than 15% risk of dying from meningitis, although the risk is higher among people âgées5.
If the doctor suspects bacterial meningitis, given the serious dangers that the patient is facing, it is imperative that initiate antibiotic treatment immediately, without waiting for test results.
The patient is sometimes treated with corticosteroids to help prevent hearing loss caused by nerve damage due to inflammatory reaction, one of the most common complications.
We will also try to prevent and treat cerebral edema by avoiding overhydration and elevating the head of bed to 30 degrees.Sometimes in cases of intracranial hypertension important, we prescribe barbiturates or mannitol.
Convalescence after meningitis can be lengthy, since it is a very serious disease which draws heavily in energy reserves of the body. Some people take several months to recover.
Depression post-meningitis would also be fairly common. It is recommended not to rush back to work and return gradually, if necessary.
Complementary
Of bacterial meningitis is a medical emergency. Any undue delay of antibiotics can lead to serious consequences, even fatal. Once reported symptoms, only antibiotics can treat meningitis.
TRAVEL WARNINGS BEFORE STARTING
The main precaution is to make the necessary vaccinations
This will depend on the destination, living conditions, health situation of the country visited and personal factors (age, vaccination status personal)
Vaccination against yellow fever (qv) is sometimes a legal requirement to pass certain boundaries.
It remains essential, and the journey can be an opportunity to update their immunizations against polio, tetanus.
Children must be current on vaccinations against measles because the disease can be very serious in some developing countries ..
In black Africa, Eastern Amazon and Southeast Asian countries with high endemicity of hepatitis B vaccine that can only be strongly recommended. (See VACCINE HEPATITIS B)
Vaccination against yellow fever is mandatory for certain countries of tropical Africa or South America.
This vaccination is performed only in accredited centers
This is a live attenuated vaccine administered as an injection at least 10 days before departure.
Its administrative validity of 10 years, but a reminder seems useful every 5 years.
For travel in a third world country or hygiene conditions are precarious, it is recommended to get vaccinated against hepatitis A in particular young people who do not yet have immunity against this vaccine virus.plusieurs exist (see hepatitis A vaccine).
Vaccination against typhoid fever may be recommended especially for foreign populations in France and returning to their country, for example on holiday.
To stay at risk of meningitis epidemic that is:
– Area African Sahel, particularly during the dry season
– North India
– Nepal
– North Vietnam
– Middle East (Saudi Arabia for the pilgrimage to Mecca)
This vaccination is carried out by administering a single injection, and protects for 4 years
such vaccination is against serogroups A and C of the disease.
To stay ‘adventurous’ in a Third World a rabies vaccination is recommended, because it is very difficult to obtain the vaccine in those countries.
Vaccinating young children to walk is also recommended.
The vaccination regimen is one injection on days 0, D7, D28, and return after one year.
A booster vaccination against diphtheria is essential to stay in Russia or Eastern Europe where a risk of epidemic of diphtheria exists.
To stay in Central Europe or North East (Austria, Czechoslovakia, Baltic States) it is recommended to be vaccinated against tick-borne encephalitis (qv)
The vaccine is not yet available in France but is the subject of a temporary use. In approved centers for vaccination against yellow fever /
Two injections a month apart are required to recall after one year.
Vaccination can be administered as young as 1 year.
For an extended stay in rural areas of Southeast Asia, China and India, it is recommended to be vaccinated against Japanese encephalitis (qv), including severe forms primarily affect children under 15 years and the elderly.
This vaccine is also the subject of a temporary authorization for use near the centers of vaccination against yellow fever.
three injections are needed at D0, D7, D28 with recall of 1 to 3 years later
Vaccination from the age of 1 year.
With regard to malaria it is necessary to refer to the many questions on this subject by typing your MALARIA Minitel.